Search
- Page Path
- HOME > Search
- Diabetes, Obesity and Metabolism
- Impact of Post-Transplant Diabetes Mellitus on Survival and Cardiovascular Events in Kidney Transplant Recipients
- Ja Young Jeon, Shin Han-Bit, Bum Hee Park, Nami Lee, Hae Jin Kim, Dae Jung Kim, Kwan-Woo Lee, Seung Jin Han
- Endocrinol Metab. 2023;38(1):139-145. Published online February 6, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1594
- 1,660 View
- 120 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Post-transplant diabetes mellitus (PTDM) is a risk factor for poor outcomes after kidney transplantation (KT). However, the outcomes of KT have improved recently. Therefore, we investigated whether PTDM is still a risk factor for mortality, major atherosclerotic cardiovascular events (MACEs), and graft failure in KT recipients.
Methods
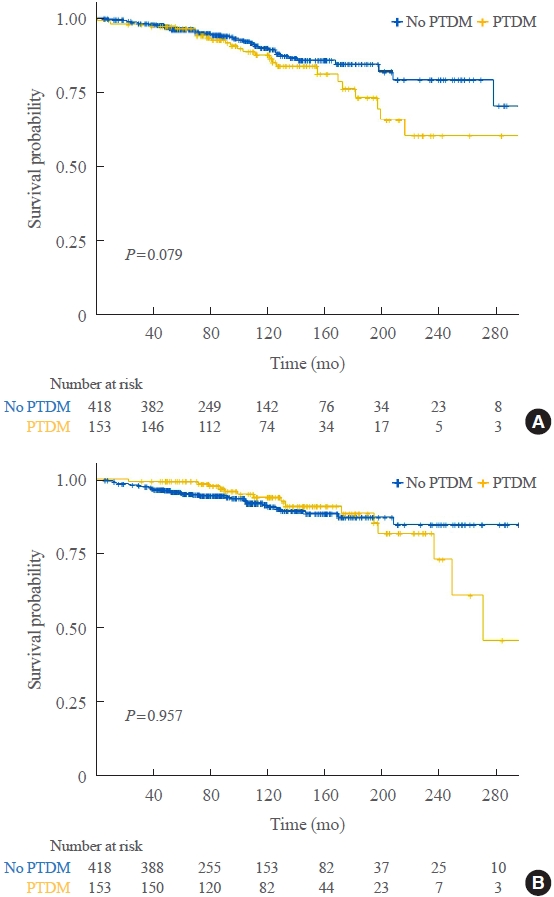
We studied a retrospective cohort of KT recipients (between 1994 and 2017) at a single tertiary center, and compared the rates of death, MACEs, overall graft failure, and death-censored graft failure after KT between patients with and without PTDM using Kaplan-Meier analysis and a Cox proportional hazard model.
Results
Of 571 KT recipients, 153 (26.8%) were diagnosed with PTDM. The mean follow-up duration was 9.6 years. In the Kaplan- Meier analysis, the PTDM group did not have a significantly increased risk of death or four-point MACE compared with the non-diabetes mellitus group (log-rank test, P=0.957 and P=0.079, respectively). Multivariate Cox proportional hazard models showed that PTDM did not have a negative impact on death or four-point MACE (P=0.137 and P=0.181, respectively). In addition, PTDM was not significantly associated with overall or death-censored graft failure. However, patients with a long duration of PTDM had a higher incidence of four-point MACE.
Conclusion
Patient survival and MACEs were comparable between groups with and without PTDM. However, PTDM patients with long duration diabetes were at higher risk of cardiovascular disease. -
Citations
Citations to this article as recorded by- Effect of post-transplant diabetes mellitus on cardiovascular events and mortality: a single‐center retrospective cohort study
Uğur Ünlütürk, Tolga Yıldırım, Merve Savaş, Seda Hanife Oğuz, Büşra Fırlatan, Deniz Yüce, Nesrin Damla Karakaplan, Cemile Selimova, Rahmi Yılmaz, Yunus Erdem, Miyase Bayraktar
Endocrine.2024;[Epub] CrossRef - Prevalence of new-onset diabetes mellitus after kidney transplantation: a systematic review and meta-analysis
Qiufeng Du, Tao Li, Xiaodong Yi, Shuang Song, Jing Kang, Yunlan Jiang
Acta Diabetologica.2024;[Epub] CrossRef - Safety and efficacy of semaglutide in post kidney transplant patients with type 2 diabetes or Post-Transplant diabetes
Moeber Mohammed Mahzari, Omar Buraykan Alluhayyan, Mahdi Hamad Almutairi, Mohammed Abdullah Bayounis, Yazeed Hasan Alrayani, Amir A. Omair, Awad Saad Alshahrani
Journal of Clinical & Translational Endocrinology.2024; 36: 100343. CrossRef
- Effect of post-transplant diabetes mellitus on cardiovascular events and mortality: a single‐center retrospective cohort study

- Clinical Study
- Apolipoprotein B Levels Predict Future Development of Hypertension Independent of Visceral Adiposity and Insulin Sensitivity
- Seung Jin Han, Wilfred Y. Fujimoto, Steven E. Kahn, Donna L. Leonetti, Edward J. Boyko
- Endocrinol Metab. 2020;35(2):351-358. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.351
- 5,814 View
- 130 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
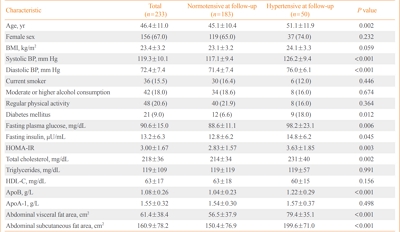
High plasma apolipoprotein B (apoB) levels have been shown to be associated with hypertension, central obesity, and insulin resistance in cross-sectional research. However, it is unclear whether apoB levels predict future hypertension independent of body composition and insulin sensitivity. Therefore, we prospectively investigated whether plasma apoB concentrations independently predicted the risk of hypertension in a cohort of Japanese Americans.
Methods
A total of 233 normotensive Japanese Americans (77 men, 156 women; mean age, 46.4±11.0 years) were followed over 10 years to monitor them for the development of hypertension. Fasting plasma concentrations of apoB, glucose, and insulin were measured at baseline. Insulin sensitivity was estimated using the homeostasis model assessment of insulin resistance (HOMA-IR). The abdominal visceral and subcutaneous fat areas were measured at baseline using computed tomography. Logistic regression analysis was used to estimate the association between apoB concentrations and the odds of incident hypertension.
Results
The 10-year cumulative incidence of hypertension was 21.5%. The baseline apoB level was found to be positively associated with the odds of incident hypertension over 10 years after adjustment for age, sex, body mass index, systolic blood pressure, abdominal visceral fat area, abdominal subcutaneous fat area, total plasma cholesterol concentration, diabetes status, and HOMA-IR at baseline (odds ratio and 95% confidence interval for a 1-standard deviation increase, 1.89 [1.06 to 3.37]; P=0.030).
Conclusion
Higher apoB concentrations predicted greater risks of future hypertension independent of abdominal visceral fat area and insulin sensitivity in Japanese Americans. -
Citations
Citations to this article as recorded by- Correlation between Central Obesity and Liver Function in Young Adults—A Cross-Sectional Study
John Alvin, Damodara Gowda KM
Journal of Health and Allied Sciences NU.2023; 13(02): 273. CrossRef - Serum amyloid A in children and adolescents: association with overweight and carotid intima-media thickness
Maria Vitória Mareschi Barbosa, João Carlos Pina Faria, Stephanie Ramos Coelho, Fernando Luiz Affonso Fonseca, Andrea Paula Kafejian Haddad, Fabíola Isabel Suano de Souza, Roseli Oselka Saccardo Sarni
einstein (São Paulo).2023;[Epub] CrossRef - The association of the apolipoprotein B/A1 ratio and the metabolic syndrome in children and adolescents: a systematic review and meta-analysis
Kayhan Dinpanah, Toba Kazemi, Sameep Shetty, Saeede Khosravi Bizhaem, Ali Fanoodi, Seyed Mohammad Riahi
Journal of Diabetes & Metabolic Disorders.2023;[Epub] CrossRef - Current Data and New Insights into the Genetic Factors of Atherogenic Dyslipidemia Associated with Metabolic Syndrome
Lăcramioara Ionela Butnariu, Eusebiu Vlad Gorduza, Elena Țarcă, Monica-Cristina Pânzaru, Setalia Popa, Simona Stoleriu, Vasile Valeriu Lupu, Ancuta Lupu, Elena Cojocaru, Laura Mihaela Trandafir, Ștefana Maria Moisă, Andreea Florea, Laura Stătescu, Minerva
Diagnostics.2023; 13(14): 2348. CrossRef - Sex-Based Differences and Risk Factors for Comorbid Nonalcoholic Fatty Liver Disease in Patients with Bipolar Disorder: A Cross-Sectional Retrospective Study
Ying Wang, Yiyi Liu, Xun Zhang, Qing Wu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3533. CrossRef - Apolipoprotein B Displays Superior Predictive Value Than Other Lipids for Long-Term Prognosis in Coronary Atherosclerosis Patients and Particular Subpopulations: A Retrospective Study
Chunyan Zhang, Jingwei Ni, Zhenyue Chen
Clinical Therapeutics.2022; 44(8): 1071. CrossRef - Genetics of Cholesterol-Related Genes in Metabolic Syndrome: A Review of Current Evidence
Sok Kuan Wong, Fitri Fareez Ramli, Adli Ali, Nurul ‘Izzah Ibrahim
Biomedicines.2022; 10(12): 3239. CrossRef
- Correlation between Central Obesity and Liver Function in Young Adults—A Cross-Sectional Study

- Clinical Study
- Obesity and Hyperglycemia in Korean Men with Klinefelter Syndrome: The Korean Endocrine Society Registry
- Seung Jin Han, Kyung-Soo Kim, Wonjin Kim, Jung Hee Kim, Yong-ho Lee, Ji Sun Nam, Ji A Seo, Bu Kyung Kim, Jihyun Lee, Jin Ook Chung, Min-Hee Kim, Tae-Seo Sohn, Han Seok Choi, Seong Bin Hong, Yoon-Sok Chung
- Endocrinol Metab. 2016;31(4):598-603. Published online December 20, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.4.598
- 5,295 View
- 35 Download
- 20 Web of Science
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this study was to investigate the prevalence of obesity in Korean men with Klinefelter syndrome (KS) and the associated risk factors for obesity and hyperglycemia.
Methods Data were collected retrospectively from medical records from 11 university hospitals in Korea between 1994 and 2014. Subjects aged ≥18 years with newly diagnosed KS were enrolled. The following parameters were recorded at baseline before treatment: chief complaint, height, weight, fasting glucose level, lipid panel, blood pressure, testosterone, luteinizing hormone, follicle-stimulating hormone, karyotyping patterns, and history of hypertension, diabetes, and dyslipidemia.
Results Data were analyzed from 376 of 544 initially enrolled patients. The rate of the 47 XXY chromosomal pattern was 94.1%. The prevalence of obesity (body mass index ≥25 kg/m2) in Korean men with KS was 42.6%. The testosterone level was an independent risk factor for obesity and hyperglycemia.
Conclusion Obesity is common in Korean men with KS. Hypogonadism in patients with KS was associated with obesity and hyperglycemia.
-
Citations
Citations to this article as recorded by- A dual-center study of predictive factors for sperm retrieval through microdissection testicular sperm extraction and intracytoplasmic sperm injection outcomes in men with non-mosaic Klinefelter syndrome
Jong Hyeun Baeck, Tae Jin Kim, Tae Heon Kim, Seung-Ryeol Lee, Dong Soo Park, Hwang Kwon, Ji Eun Shin, Dong Hyeon Lee, Young Dong Yu
Investigative and Clinical Urology.2023; 64(1): 41. CrossRef - Cardiorespiratory fitness in adolescents and young adults with Klinefelter syndrome – a pilot study
Julia Spiekermann, Kathrin Sinningen, Beatrice Hanusch, Michaela Kleber, Michael M. Schündeln, Cordula Kiewert, Heide Siggelkow, Jakob Höppner, Corinna Grasemann
Frontiers in Endocrinology.2023;[Epub] CrossRef - Metabolic Profile in a Cohort of Young Sicilian Patients with Klinefelter’s Syndrome: The Role of Irisin
Stefano Radellini, Valentina Guarnotta, Vincenzo Sciabica, Giuseppe Pizzolanti, Carla Giordano, Vito Angelo Giagulli
International Journal of Endocrinology.2022; 2022: 1. CrossRef - Metabolic and Nutritional Aspects in Paediatric Patients with Klinefelter Syndrome: A Narrative Review
Chiara Mameli, Giulia Fiore, Arianna Sangiorgio, Marta Agostinelli, Giulia Zichichi, Gianvincenzo Zuccotti, Elvira Verduci
Nutrients.2022; 14(10): 2107. CrossRef - Klinefelter syndrome in an adolescent with severe obesity, insulin resistance, and hyperlipidemia, successfully treated with testosterone replacement therapy
Shota Fukuhara, Jun Mori, Hisakazu Nakajima
Clinical Pediatric Endocrinology.2021; 30(3): 127. CrossRef - Glucose metabolic disorder in Klinefelter syndrome: a retrospective analysis in a single Chinese hospital and literature review
Shixuan Liu, Tao Yuan, Shuoning Song, Shi Chen, Linjie Wang, Yong Fu, Yingyue Dong, Yan Tang, Weigang Zhao
BMC Endocrine Disorders.2021;[Epub] CrossRef - What Every Internist-Endocrinologist Should Know about Rare Genetic Syndromes in Order to Prevent Needless Diagnostics, Missed Diagnoses and Medical Complications: Five Years of ‘Internal Medicine for Rare Genetic Syndromes’
Anna G. W. Rosenberg, Minke R. A. Pater, Karlijn Pellikaan, Kirsten Davidse, Anja A. Kattentidt-Mouravieva, Rogier Kersseboom, Anja G. Bos-Roubos, Agnies van Eeghen, José M. C. Veen, Jiske J. van der Meulen, Nina van Aalst-van Wieringen, Franciska M. E. H
Journal of Clinical Medicine.2021; 10(22): 5457. CrossRef - Klinefelter Syndrome and Diabetes
Mark J. O’Connor, Emma A. Snyder, Frances J. Hayes
Current Diabetes Reports.2019;[Epub] CrossRef - Endocrine aspects of Klinefelter syndrome
Adriana Herrera Lizarazo, Michelle McLoughlin, Maria G. Vogiatzi
Current Opinion in Endocrinology, Diabetes & Obesity.2019; 26(1): 60. CrossRef - Sex differences in metabolism and cardiometabolic disorders
Karthickeyan Chella Krishnan, Margarete Mehrabian, Aldons J. Lusis
Current Opinion in Lipidology.2018; 29(5): 404. CrossRef - Klinefelter Syndrome: Integrating Genetics, Neuropsychology, and Endocrinology
Claus H Gravholt, Simon Chang, Mikkel Wallentin, Jens Fedder, Philip Moore, Anne Skakkebæk
Endocrine Reviews.2018; 39(4): 389. CrossRef - Sex differences in obesity, lipid metabolism, and inflammation—A role for the sex chromosomes?
Temeka Zore, Maria Palafox, Karen Reue
Molecular Metabolism.2018; 15: 35. CrossRef - Klinefelter syndrome, insulin resistance, metabolic syndrome, and diabetes: review of literature and clinical perspectives
Andrea Salzano, Roberta D’Assante, Liam M. Heaney, Federica Monaco, Giuseppe Rengo, Pietro Valente, Daniela Pasquali, Eduardo Bossone, Daniele Gianfrilli, Andrea Lenzi, Antonio Cittadini, Alberto M. Marra, Raffaele Napoli
Endocrine.2018; 61(2): 194. CrossRef - Síndrome de Klinefelter y riesgo cardiovascular
A. Yamaguchi, P. Knoblovits
Hipertensión y Riesgo Vascular.2018; 35(4): 195. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Sex differences in obesity: X chromosome dosage as a risk factor for increased food intake, adiposity and co-morbidities
Karen Reue
Physiology & Behavior.2017; 176: 174. CrossRef - Klinefelter Syndrome with Morbid Obesity Before Bariatric Surgery: A Case Report
Parisa Janmohammadi, Gholamreza Mohammadi-Farsani, Hana Arghavani, Mahmoud Arshad, Tayebeh Mokhber
Journal of Minimally Invasive Surgical Sciences.2017;[Epub] CrossRef - Klinefelter Syndrome and Metabolic Disorder
Ji Cheol Bae
Endocrinology and Metabolism.2016; 31(4): 535. CrossRef
- A dual-center study of predictive factors for sperm retrieval through microdissection testicular sperm extraction and intracytoplasmic sperm injection outcomes in men with non-mosaic Klinefelter syndrome

- A Case of an Adrenocortical Carcinoma with Pulmonary Embolism as the Initial Manifestation.
- Hyo Jin Lee, Ji Young Kwak, Young Jip Kim, Tae Ho Kim, Jan Dee Lee, Hyun Woo Lee, Hae Jin Kim, Dae Jung Kim, Yoon Sok Chung, Kwan Woo Lee, Seung Jin Han
- Endocrinol Metab. 2012;27(1):93-97. Published online March 1, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.1.93
- 1,962 View
- 26 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - The annual incidence of a first episode of deep vein thrombosis or pulmonary embolism (PE) in the general population is 120 per 100,000. Cancer is associated with an approximately 4- to 7-fold higher risk of thrombosis. Adrenocortical carcinoma (ACC) is a rare type of malignancy, accounting for 0.02% of all cancers reported annually. Approximately 40% of ACCs are nonsecretory. Most patients with nonsecreting tumors have clinical manifestations related to tumor growth (e.g., abdominal or flank pain). Often the adrenal mass is detected by chance via radiographic imaging. As a result, most ACC patients are diagnosed at an advanced stage and have a poor prognosis. Herein, we report a case of a 54-year-old woman who was admitted to our emergency department complaining of dyspnea. She was diagnosed with ACC accompanied by thrombi in the pulmonary artery and inferior vena cava. We performed a left adrenalectomy and administered adjuvant radiotherapy. The patient is currently receiving warfarin and adjuvant mitotane therapy. She was incidentally diagnosed with ACC, with PE as the initial manifestation.
-
Citations
Citations to this article as recorded by- Iliac vein deep vein thrombosis as an atypical presentation of an adrenocortical carcinoma
Arshpreet Singh Badesha, Taha Khan, Engy Abdellatif
BMJ Case Reports.2022; 15(5): e248708. CrossRef
- Iliac vein deep vein thrombosis as an atypical presentation of an adrenocortical carcinoma

- A Case of Persistent Hyperkalemia After Unilateral Adrenalectomy for Aldosterone-Producing Adenoma.
- Min Jae Yang, Seung Jin Han, Min Seok Lee, Eun Kyung Kim, Hae Jin Kim, Dae Jung Kim, Yoon Sok Chung, Tae Hee Lee, Jang Hee Kim, Kwan Woo Lee
- J Korean Endocr Soc. 2009;24(3):201-205. Published online September 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.3.201
- 1,871 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Primary aldosteronism is a syndrome characterized by various clinical features that are due to excessive autonomous aldosterone secretion not sustained by the activation of the renin-angiotensin system. Aldosterone-producing adrenal adenoma is found in approximately 35% of the patients who suffer with primary aldosteronism. Laparoscopic adrenalectomy is the standard treatment for aldosterone-producing adrenal adenoma, and the result of this operation is normalization of the serum potassium and plasma aldosterone concentrations, as well as correcting the plasma renin activity in most cases. However, it is known that some of the patients with aldosterone-producing adrenal adenoma show transient hyperkalemia postoperatively due to the reversible suppression of the renin-aldosterone axis. We recently experienced the case of a 54-year-old woman with an aldosterone-producing adrenal adenoma, and she presented with severe hyperkalemia after unilateral adrenalectomy. Compared with the previously reported cases that showed transient suppression of the rennin-aldosterone axis for less than 7 months, our patient revealed a prolonged episode of hyperkalemia for 8 months postoperatively, and this required continuous mineralocorticoid replacement.

- Pituitary Hormonal Changes after Transsphenoidal Tumor Removal in Non-Functioning Pituitary Adenoma.
- Min Suk Lee, Seung Jin Han, Eun Kyung Kim, Joo An Hwang, Yoon Sok Chung, Se Hyuk Kim, Kyung Gi Cho, Nae Jung Rim, Ho Sung Kim
- J Korean Endocr Soc. 2009;24(3):181-188. Published online September 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.3.181
- 1,663 View
- 22 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The present study investigated the rates and the potential predictors of either new pituitary loss or recovery of hormonal function after transsphenoidal removal of a non-functioning pituitary adenoma. METHODS: Patients who underwent transsphenoidal removal of a non-functioning pituitary adenoma from January 2003 to December 2007 at Ajou University Medical Center were included in this retrospective analysis. Patients were excluded if they had a history of previous pituitary tumor surgery, or did not have preoperative pituitary hormonal data. RESULTS: Of 42 patients included in the analysis, 36 patients had hypopituitarism, 21 patients had "stalk compression" hyperprolactinemia, and 2 patients had normal pituitary function. At long term follow-up (longer than 6 months), 13 patients showed postoperative pituitary hormonal recovery in at least 1 hormonal axis, while 6 patients had developed postoperative hormonal loss in at least 1 hormonal axis. On analysis, neither preoperative serum prolactin level nor tumor size was related to postoperative pituitary hormonal changes. CONCLUSION: More than 1/3 of patients who underwent transsphenoidal surgery showed postoperative pituitary hormonal recovery. -
Citations
Citations to this article as recorded by- Childhood Onset Pituitary Adenoma: Clinical Presentations and Outcomes of 24 Cases
Hwa Young Kim, Hae Woon Jung, Jieun Lee, Ju Young Yoon, Young Ah Lee, Choong Ho Shin, Sei Won Yang
Annals of Pediatric Endocrinology & Metabolism.2012; 17(2): 82. CrossRef
- Childhood Onset Pituitary Adenoma: Clinical Presentations and Outcomes of 24 Cases

- A Case of Panhypopituitarism and Central Diabetes Insipidus Caused by Primary Central Nervous System Lymphoma.
- Mi Sun Ahn, Soon Sun Kim, Tae Ho Kim, Seung Jin Han, Dae Jung Kim, Hugh Chul Kim, Se Hyuk Kim, Jae Ho Han, Ho Sung Kim, Yoon Sok Chung
- J Korean Endocr Soc. 2008;23(4):260-265. Published online August 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.4.260
- 1,733 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Primary central nervous system (CNS) lymphoma is an uncommon neoplasm. However, the incidence of primary CNS lymphoma has increased more than 10-fold over the past three decades, and continues to accelerate. Currently, primary CNS lymphoma represents 4 to 7 percent of all newly diagnosed primary CNS tumors. Primary CNS lymphoma may arise from different parts of the brain, with deep hemispheric periventricular white matter being the most common site of origin. The presenting symptoms in primary CNS lymphoma vary depending on the location of the mass. Involvement of the hypothalamic-pituitary axis may cause hypopituitarism, diabetes insipidus, headache, diplopia, and blurred vision.

- Non-functional Pituitary Adenoma Detected on (18)F-fluorodeoxyglucose Positron Emission Tomography ((18)F-FDG-PET) in a Patient with Mucosa-associated Lymphoid Tissue Lymphoma.
- Jin Ha Lee, Seung Jin Han, Se Eun Park, Mi Ae Cho, June Won Cheong, Mijin Yun, Yumie Rhee, Eun Jig Lee, Sung Kil Lim
- J Korean Endocr Soc. 2008;23(2):137-141. Published online April 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.2.137
- 1,816 View
- 19 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Magnetic resonance imaging (MRI) is the modality of choice for the detection and characterization of a pituitary adenoma. Uptake of (18)F-fluorodeoxyglucose (FDG) by intrasellar tumors, including pituitary adenomas, has been reported in several previous studies. We report a case where a pituitary adenoma was detected on FDG-positron emission tomography (PET), but the tumor was not detected with the use of sellar MRI. A 31-year-old woman was referred to the clinic due to a focal increase of FDG uptake at the pituitary fossa seen on whole body FDG-PET. The patient was receiving chemotherapy due to a recurred B-cell lymphoma of the mucosa-associated lymphoid tissue type. Subsequently, sellar MRI was performed, and images showed a small non-enhancing heterogenous cystic lesion in the midline of the pituitary gland, radiologically suggestive of a Rathke's cleft cyst. However, sellar MRI failed to identify a lesion consistent with a pituitary tumor that corresponded to the site of increased FDG uptake detected by the use of PET, despite the inclusion of a dynamic contrast enhanced sequence. Despite the negative findings of the MRI examination, basal and stimulated levels of the GnRH free alpha-subunit were profoundly increased. Therefore, we suspected the presence of a non-functional pituitary tumor in addition to a Rathke's cleft cyst, rather than pituitary involvement of a lymphoma, based on the hormone levels and PET scan findings.
-
Citations
Citations to this article as recorded by- Clinical Characteristics of 16 Patients with Pituitary Tumor Incidentally Detected by18F-Fluorodeoxyglucose PET-CT (18F-FDG PET-CT)
Hyung Jin Kim, Gi Jeong Cheon, A Ra Cho, Chang Hoon Lee, Sang Min Youn, Se jin Ahn, Sang Eon Jang, Jung Min Kim, Yun Yong Lee, Ka Hee Yi
Endocrinology and Metabolism.2010; 25(4): 321. CrossRef
- Clinical Characteristics of 16 Patients with Pituitary Tumor Incidentally Detected by18F-Fluorodeoxyglucose PET-CT (18F-FDG PET-CT)

- A Case of Multiple Endocrine Neoplasia Type 1 with Mutation in MENIN Gene.
- Se Eun Park, Eun Seok Kang, Hyun Joo Lee, So Hun Kim, Mi Young Do, Shin Ae Kang, Seung Jin Han, Hyeong Jin Kim, Chul Woo Ahn, Bong Soo Cha, Sung Kil Lim, Kyung Rae Kim, Il Jin Kim, Hyun Chul Lee
- J Korean Endocr Soc. 2005;20(1):71-77. Published online February 1, 2005
- DOI: https://doi.org/10.3803/jkes.2005.20.1.71
- 2,046 View
- 22 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - Multiple endocrine neoplasia type 1(MEN 1) is an autosomal dominantly inherited syndrome, characterized by the combined occurrence of tumors of the parathyroid glands, endocrine pancreas, and anterior pituitary gland. The MENIN gene, which is a kind of tumor suppressor gene, is located at the chromosomal locus 11q13. It consists of one untranslated exon and nine exons encoding the menin protein. We report a case of a 22-yearss-old woman with MEN type 1, who was proven to have a mutation in the MENIN gene. The patient was admitted because of repeated hypoglycemia. The fasting plasma glucose level was 32mg/dL. Seventy two hours fasting test showed an the insulin/glucose ratio as 0.33. Endoscopic ultrasonography detected multiple masses on the pancreas. The arterial -stimulated venous sampling(ASVS) with calcium showed sudden step up of insulin at the head and tail portions of the pancreas. The sellar MRI showed a pituitary mass that produced prolactin. Instead of a pathologic diagnosis from operational specimen, the genetic analysis revealed a mutation in the MENIN 1 gene(exon 2, 200~201insAGCCC).
-
Citations
Citations to this article as recorded by- Genetic and Epigenetic Analysis in Korean Patients with Multiple Endocrine Neoplasia Type 1
Yoon Jung Chung, Sena Hwang, Jong Ju Jeong, Sun Yong Song, Se Hoon Kim, Yumie Rhee
Endocrinology and Metabolism.2014; 29(3): 270. CrossRef - A Case of Familial Multiple Endocrine Neoplasia Type 1 with a Novel Mutation in theMEN1Gene
Min Jung Kim, Eun Hee Kim, Mi-Seon Shin, Joo Hui Kim, Hee Kyung Na, Seong Joon Park, Sang Ah Lee, Eun Hee Koh, Woo Je Lee, Ki Ho Song, Joong-Yeol Park, Ki-Up Lee, Gu-Hwan Kim, Han-Wook Yoo, Min-Seon Kim
Endocrinology and Metabolism.2011; 26(2): 171. CrossRef - Somatic Mutational Analysis of MEN1 and Phenotypic Correlation in Sporadic Parathyroid Tumors
Young Su Chae, Hee Jin Kim, Sun Wook Kim, Myung-Chul Chang
Journal of the Korean Surgical Society.2009; 76(1): 15. CrossRef - Multiple Endocrine Neoplasia Type 1 with Multiple Leiomyomas Linked to a Novel Mutation in the MEN1 Gene
Heekyoung Choi, Sehyun Kim, Jae-Hoon Moon, Yoon Hee Lee, Yumie Rhee, Eun Seok Kang, Chul Woo Ahn, Bong Soo Cha, Eun Jig Lee, Kyung Rae Kim, Hyun Chul Lee, Seon Yong Jeong, Hyun Ju Kim, Sung-Kil Lim
Yonsei Medical Journal.2008; 49(4): 655. CrossRef - A Case of Familial Multiple Endocrine Neoplasia Type 1 with MEN1 Gene Mutation
Young Eun Jo, Yong-Jun Choi, Yun Kyung Kim, Sang Mi Ahn, Sun Hye Jung, Hae Jin Kim, Dae Jung Kim, Kwan Woo Lee, Ji-Hee Hong, Seon-Yong Jeong, Hyon J Kim, Yoon-Sok Chung
Journal of Korean Endocrine Society.2007; 22(1): 68. CrossRef - A Case of Familial Multiple Endocrine Neoplasia with MEN1 Gene Mutation
Hye-Young Sung, Yeon-Joo Chun, Hyeug Lee, Bum Jun Kwon, Kun Woo Park, Jung Min Lee, Sung Dae Moon, Sang Ah Chang, Je-Ho Han
Journal of Korean Endocrine Society.2006; 21(6): 560. CrossRef
- Genetic and Epigenetic Analysis in Korean Patients with Multiple Endocrine Neoplasia Type 1

- Adiponectin Gene Polymorphism and Carotid Artery Intima-Media thickness in Type 2 Diabetes.
- Eun Seok Kang, So Young Park, So Hun Kim, Hyun Joo Lee, Kyu Yeon Hur, Seung Jin Han, Se Eun Park, Hyeong Jin Kim, Chul Woo Ahn, Bong Soo Cha, Sung Kil Lim, Kyung Rae Kim, Hyun Chul Lee
- J Korean Endocr Soc. 2005;20(1):29-39. Published online February 1, 2005
- DOI: https://doi.org/10.3803/jkes.2005.20.1.29
- 1,781 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The aim of this study was to examine the association between the common polymorphisms of the adiponectin gene(ACDC) and the intima-media thickness(IMT) of the common carotid arteries in type 2 diabetic patients. METHODS: The B mode ultrasound examination of carotid artery was performed on 133 type 2 diabetic patients. The carotid IMT was calculated using the Intimascope computer program. The SNP45 and SNP276 of the ACDC were examined. RESULTS: There was no significant difference in the carotid IMT among the SNP45 genotypes(0.66+/-0.18mm for TT, 0.71+/-0.12mm for TG and 0.64+/-0.15mm for GG, P=NS). Subjects carrying the SNP276 GG genotype had a markedly lower serum adiponectin concentration than those carrying the TT genotype(3.35+/-2.00microgram/mL vs. 4.98+/-2.24microgram/mL, P=0.029) The carotid IMT was significantly higher in patients with the SNP276 GG genotype than those with the TT genotype (0.70+/-0.17mm vs. 0.59+/-0.13mm, P=0.032). Patients with the +45GG/+276GG genotype combination showed significantly higher mean carotid IMT than the other genotype combinations(0.78+/-0.09mm vs. 0.71+/-0.15mm, P=0.013) CONCLUSIONS: These results suggest that the adiponectin gene, SNP276 is associated with the carotid IMT in type 2 diabetic patients. Further studies are will be needed to confirm these genotypephenotype associations.


 KES
KES

 First
First Prev
Prev



